Healthcare IT Is Not a Checkbox: Why Compliance-Only Security Fails
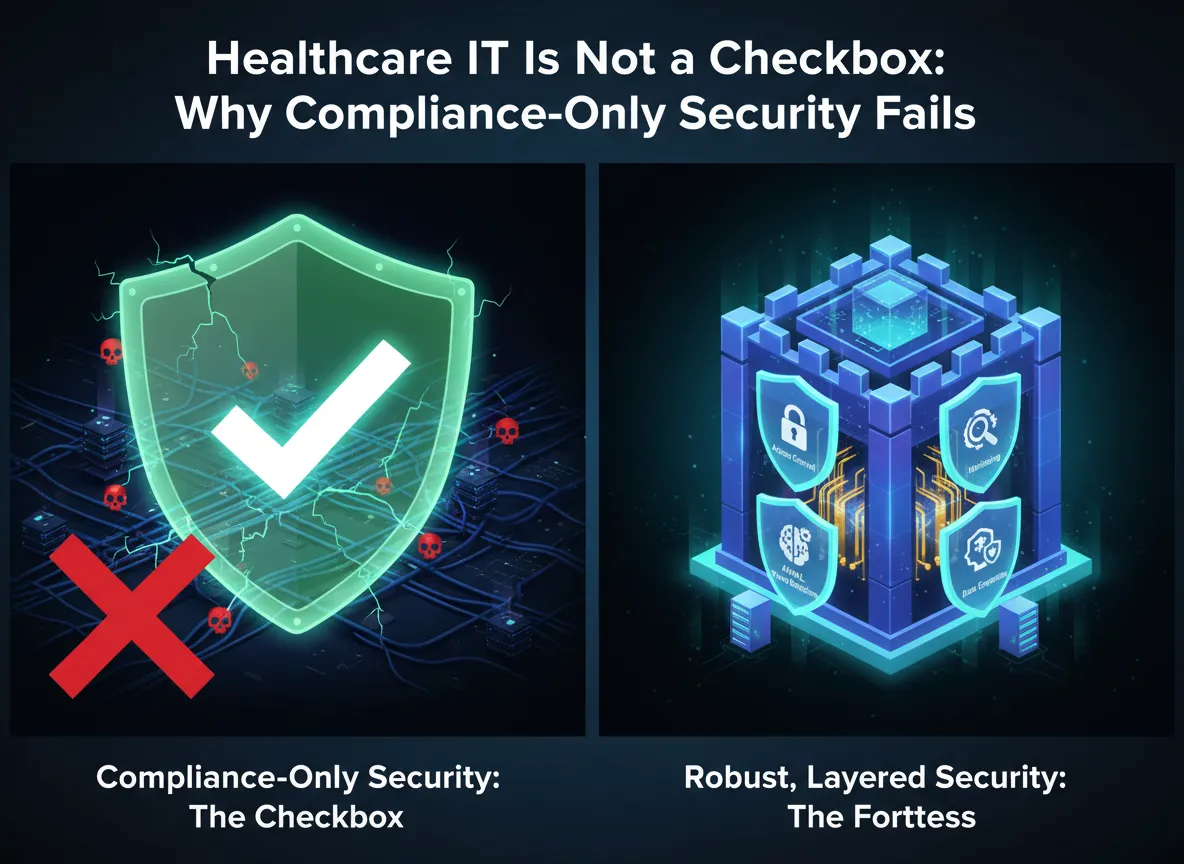
In healthcare, I no longer view information technology as a background utility. It is a core clinical and operational system. Electronic health records, imaging platforms, patient portals, billing systems, and connected medical devices directly affect patient care, safety, and regulatory compliance. Yet I still see many organizations treating Healthcare IT as a “check-the-box” exercise, doing the bare minimum to satisfy audits, insurers, or regulators.
That mindset is increasingly risky.
Regulators, attackers, and patients now expect healthcare organizations to treat IT and cybersecurity as mission-critical functions. When Healthcare IT is reduced to compliance theater, the outcomes are often predictable and severe: ransomware outages, data breaches, patient safety events, regulatory penalties, and long-term reputational damage.
Why “Check-the-Box” Healthcare IT Fails
When I assess environments that rely on checkbox compliance, I see the same patterns repeatedly. Annual HIPAA risk assessments are completed but never updated or remediated. Security policies exist primarily for auditors and are rarely followed in day-to-day operations. Backup systems look acceptable on paper but have never been tested. Clinical systems run on outdated hardware and unsupported operating systems. Staff training is limited to a once-a-year video with no reinforcement. IT decisions are driven by cost avoidance instead of risk management.
These organizations may appear compliant on paper, but in reality they are often one incident away from operational paralysis.
Why Healthcare IT Requires a Higher Standard
Healthcare IT deserves a higher standard because patient care depends on it. When EHRs, lab systems, imaging platforms, or scheduling tools go down, providers revert to manual workflows, clinical decisions slow, medication errors become more likely, and patient throughput drops sharply. I have seen ransomware incidents force clinics to cancel appointments, divert patients, or operate with limited visibility. Treating IT as an afterthought ignores its direct impact on patient safety.
Regulators also expect more than documentation. In enforcement actions, I consistently see scrutiny focused on whether risk analyses are current and accurate, whether identified risks were actually mitigated, whether security controls function in practice, whether incident response plans work under pressure, and whether backups and recovery processes are tested. Organizations that cannot demonstrate real, ongoing security management face fines, corrective action plans, and extended oversight, regardless of how many policies they have on file.
Cybercriminals further exploit minimal-effort environments. Healthcare remains a prime ransomware target precisely because many organizations are underfunded, understaffed, and under-protected. Attackers look for unpatched systems, weak remote access, poor email security, flat networks, limited monitoring, and backups that can be deleted or encrypted. A checkbox IT program creates predictable weaknesses that adversaries exploit efficiently.
What Taking Healthcare IT Seriously Actually Looks Like
When I work with organizations that take Healthcare IT seriously, I see a clear shift from avoidance to management of risk. Risk analysis becomes a living process, not an annual task. Risks are prioritized based on likelihood and impact, remediation is tracked with accountability, and controls evolve as systems, vendors, and threats change.
Security controls are enforced operationally, not just documented. Multifactor authentication protects email, EHRs, VPNs, and administrative accounts. Endpoint detection and response is deployed and monitored. Networks are segmented to separate clinical, administrative, and guest systems. Cloud platforms are configured securely. Vulnerability management and patching are routine, not reactive. If a control cannot be verified, monitored, and enforced, I do not consider it a real control.
Backup and recovery capabilities are treated as operational necessities. I assume systems will fail or be attacked, and I plan accordingly. That means independent and immutable backups, clearly defined recovery time and recovery point objectives, regular restore testing, documented downtime procedures, and alignment between IT recovery plans and clinical workflows. Backups that have never been tested are assumptions, not safeguards.
Vendor accountability is also essential. Modern healthcare environments depend on EHR vendors, MSPs, billing companies, cloud platforms, and specialty applications. Taking IT seriously means performing due diligence before onboarding vendors, requiring security and breach notification obligations in contracts, understanding exactly which vendors access protected health information, and reviewing vendor security posture on an ongoing basis. Third-party failures quickly become your operational and compliance problem.
Finally, I emphasize culture and ownership. Healthcare IT is not solely the responsibility of the IT department. Effective programs include regular, role-appropriate training, phishing simulations with follow-up education, clear reporting mechanisms, engaged executive and clinical leadership, and defined ownership for IT risk decisions. When leadership treats IT as critical, staff behavior follows.
Why the Cost of Minimal Effort Keeps Rising
Across the healthcare sector, I see larger breach penalties, longer investigations, stricter cyber insurance requirements, increased scrutiny from patients and partners, and greater operational disruption following incidents. Organizations that treat Healthcare IT as a compliance checkbox often spend far more recovering from incidents than they would have spent building a mature, proactive program.
Conclusion: Minimum Effort Is No Longer Defensible
Healthcare IT is not an administrative burden. I view it as a patient care system, a compliance system, and a business continuity system. Checkbox compliance may satisfy short-term audits, but it leaves organizations exposed to long-term clinical, legal, and operational risk. Organizations that take Healthcare IT seriously, investing in real controls, real testing, and real accountability, are more resilient, more compliant, and better positioned to deliver safe, uninterrupted care. If you are unsure whether your current approach goes beyond appearances and actually reduces risk, I encourage you to contact me for a consultation so we can assess where gaps exist and build a program that stands up in real-world conditions, not just on paper.

